The other day someone showed a photo of an angry person with the caption of a neurosurgeon responding to the complaint of the neurological status of his patient. Since the days of the pioneers of neurosurgery including Harvey Cushing we as a specialty have always struggled to prove our relevance and necessity to society. Among our medical colleagues they often feel sympathy for our hard work but doubt that it really helps most of our patients. Similarly the public often views us at times heroically or other times seriously impotent to treat hopeless conditions.
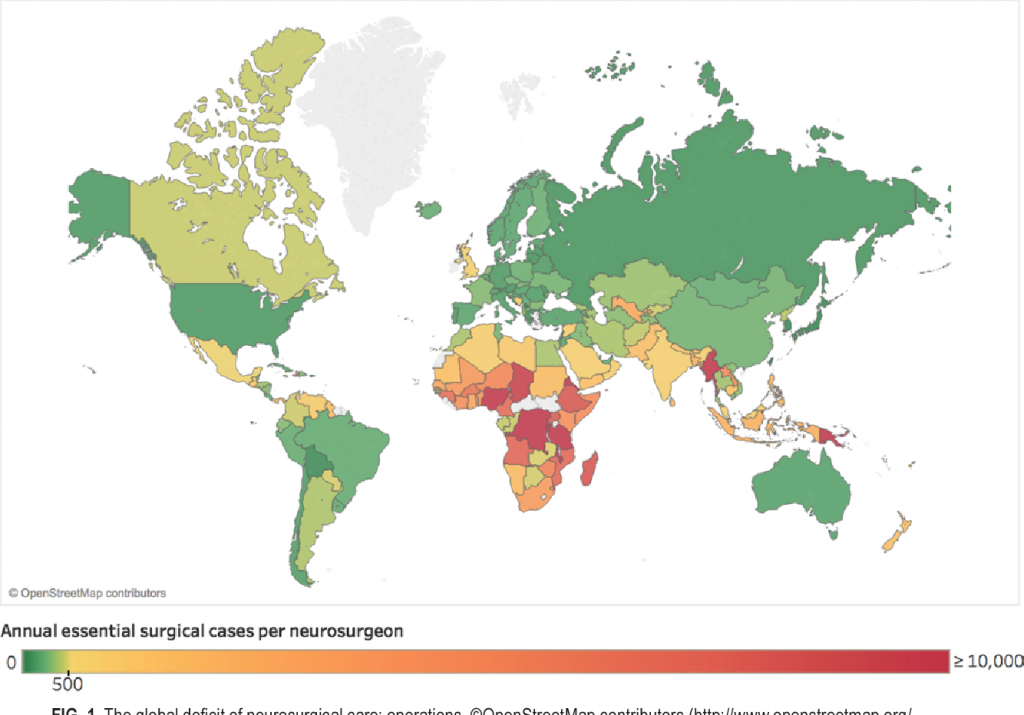
In 2018 a global survey of neurosurgery (see the enclosed photo)showed growing around the world and even in developing countries. This is a good thing. At the same time over the past several decades there has been increasing emphasis from stakeholders and political authorities for medical providers to show the effectiveness of their work and costs. What doctors do is now called relative value units and it is matched against assigned niches for our small specialty in health care budgets (both public and private).
Since I was resident about 40 years ago wonderful developments have occurred such as MRI, intravascular intervention for aneurysm, spinal instrumentation, computerized navigation, endoscopic procedures etc. As a resident we are fascinated by these wonders and the science behind them but then when residency is over we do have to make our way in the real world. It is easy and totally understandable to be drawn to lucrative fields especially spine surgery as I was because it offers frankly good rewards for hard work as well as being so ubiquitous in the population. Unfortunately it is also the field most rift with poor science and loose surgical indications such that many of our medical colleagues tend to look down upon those whose career mostly deals with this field.
The enthusiasm for complicated cases of the brain and head injury treatment often wane as one passes from the academic training environment to the realm of sustaining oneself in the world which is understandable. In discussing this I am not passing any judgment just reflecting upon a fact of life.
My advice to young neurosurgeons including my residents and fellows as well as especially those developing their careers in countries where neurosurgery is relatively new is to try to balance your contributions to society with your own financial rewards. Stay involved in teaching and research. Joining with public health officials in documenting the needs of traffic and accident victims will make society see the need for advancing neurosurgical care. Cooperate with fellow neurosurgeons and the medical community to educate stakeholders and public about how emergency care and neurosurgical centers (including trauma centers) can save so many who will continue to lead productive lives. Promote professional standards about spine care and be wary of becoming too entwined in the medical legal system. During surgery on patients who are not a risk of neurological deterioration but are likely to continue to be chronic pain sufferers does not improve your reputation or that of your profession. Let neurosurgery be the light of your medical community.