A fundamental difference in the immunity of men and women is leading to research in how a difference in response of the immune system to SARS-CoV-2 can be life saving or deadly.
Even though women contract COVID 19 more often then men in part because women outnumber men in jobs like nursing, teaching, cleaning, etc. where there is frequent interaction with large groups or areas of people they do not seem to get as seriously sick or die as often. The same phenomena was seen with previous epidemics involving different coronaviruses then the current SARS-CoV-2.
Although at first differences in smoking or hygienic practices between the sexes were considered, the evidence did not confirm this hypothesis.
The male and female sex have significant differences in their immune systems relating to the X chromosome. Females have two X chromosomes while males have one X and one Y normally. On the X chromosome are a group of genes for Toll-Like Receptors (TLR). The TLR are located in organs which are very active in immune responses to fight infection including the spleen and white blood cells as well as those with exposure to contaminants outside the body including the lungs and gastrointestinal tract. Humans have ten different TLRs labeled TLR 1 to 10. Some of the TLR (TLR 2 and 5) are specifically sensitive to bacteria while TLR 3 and 4 may be sensitive to viral antigens.
Stimulation of TLRs can cause two reactions. For most except TLR3 one reaction results in the production of cytokines which are powerful inducers of inflammatory responses affecting multiple organs. Previous coronavirus epidemics and the the current COVID 19 have been seen in some patients to cause a cytokine storm syndrome (CSS). A cascade of reactions occurs leading to severe destructive inflammation affecting the lungs, heart, kidneys and even sometimes the brain to varying degrees. Organ failure, hemodynamic instability, and ultimately death can occur. The other reaction is to stimulate interferon beta which causes macrophages to engulf antigens (invaders or under some circumstance human ) and activates a form of T-Cells called Natural Killers.
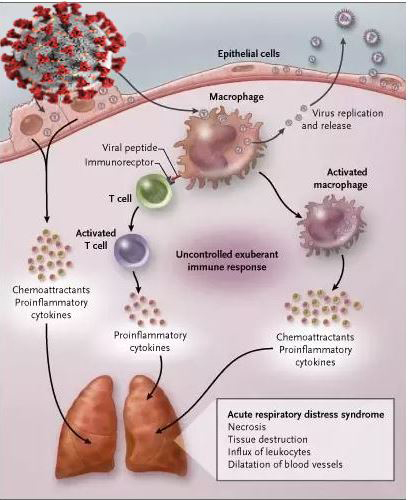
These reactions can be exaggerated causing damage to normal organs or early on may be protective. Research in mice in 2015 showed that stimulating TLR3 could create a protective response to a coronavirus.
Now getting back to the differences between the sexes. Women generally have two sets of TLRs in the body with two different gene types while men have one. Although most of the cells in the woman will randomly choose one set to be active which could be either gene this means in whole body some cells of each type will be present. Sometimes both chromosomes are working creating an approximately 15% higher level of TLR function than normal. It is suggested by some that having this situation at the time of infection may give women more protection then men as a group statistically.
The problem is that it is well known that women suffer more severely than men from chronic inflammatory conditions such as systemic lupus erythematosus. The interaction of TLRs with normal human tissues to which they become sensitized is being researched. Why do women not have a worse reaction leading to cytokine storm and more frequent death than men? Why do women do better? Could it be that having higher levels at the beginning and of two different types is important?
The controversial drug, hydroxychloroquine inhibits TLR4 response to lipopolysaccharide which in vitro studies suggest can inhibit the virus entering the membrane of the intended cell target. However when given to very sick patients resulted in worsening of lung function. Thus now it is being considered more for prophylaxis than treatment by some.
Some researchers have said that TLRS are “double edged swords” that can cure or kill. How TLRs responses are regulated and when in the course of disease these reactions are therapeutically manipulated may determine if these interventions are helpful or harmful. Research is needed how to better control them to treat COVID 19, autoimmune diseases, and even cancer.