This a review of some of the principals I follow when performing myelomeningocoel surgery in young infants in Northern Ethiopia. More than a third of all the neurosurgery operations is made up by this pediatric neurosurgical condition at our hospital.
It is estimated by the World Health Organization that over 300,000 children suffer neural tube defects which results in improper formation of the spinal cord, spine, and brain leading to absence of bowel, bladder, and sexual function control, spinal deformity, reduced mental development, and paralysis. More common in underdeveloped countries then in developed countries, the occurrence has been mostly strongly related to preconception maternal folate deficiency and some genetic factors. Unfortunately in Ethiopia there are thousands of these children born every year, we see several a week in our clinic at Ayder Comprehensive Specialized Hospital at the Mekelle University College of Health Sciences in Northern Ethiopia.
Myelomeningocoel is a disorder where the neural tube which develops in the first month after conception from a flat plate of specialized tissue fails to fully close into a tube. This results in neural elements being exposed directly to the atmosphere or only a thin membranous layer. The lowest nerves below the defect often do not completely form leading to paralysis in the lower extremities and difficulties with the functions normally performed by the sacral nerve roots involving the bladder, rectum, and sexual organs.
Pre-Operative Assessment
Pre-operatively many of these children come to the hospital from long distances in poor nutritional condition. If they weigh less than 3 kilograms we delay surgery until they reach this weight because of problems with temperature control in the operative and immediate post-operative period. Children who have cerebrospinal fluid leaks, chronic bleeding from the neural placode, progressive macrocephaly, symptomatic hydrocephalus, symptomatic Arnold-Chiari symptoms such as weak cry, weak upper extremities or multiple pneumonias from aspiration, or meningitis are given priority. Because of the large number of cases and limited resources there is often a several month waiting period for those in stable condition with well epithelialized neural tube defects.
To undergo surgery they must be fit for general anesthesia with normal hemoglobin, kidney function, cardiovascular status and be free of active infection. Ultrasound evaluations of the head to assess for hydrocephalus and of the abdomen to assess the kidneys is routinely done.
They are kept nothing per oral (NPO) for several hours before surgery and started on pediatric maintenance intravenous fluid containing glucose during this time which is continued in the operating room and after until the child is breast-feeding normally.
We do not routinely prepare blood for the surgery unless the child has a low hemoglobin/hematocrit preoperatively. If so then a pre-operative transfusion will be given.
Surgery
The child is placed under general inhalation anesthesia using isofluorane rather then halothane is the most common anesthetic agent used in Ethiopia. We use a electric heater in the room, warm the saline irrigation used during the case, intravenous fluid heaters, and keep the child covered as much as possible to avoid hypothermia which can occur easily in our mountain environment.
Pre-operative ceftriazone at 50mg/kg is given for prophylaxis and continued for 48 hours post-operatively. This is given not just to prevent wound infection but also because these children are at risk of developing post operative pneumonia from the co-existing Arnold-Chiari malformation also present.

The child is placed in prone position with an intravenous fluid bag under the chest and under the groin which leaves the abdomen free of pressure thus reducing venous bleeding during the surgery. In the picture is seen a child with a large membranous lumbar myelomeningocoel. The large size taking up most of the width of the back and the mostly membranous covering predicts that closure will be difficult.
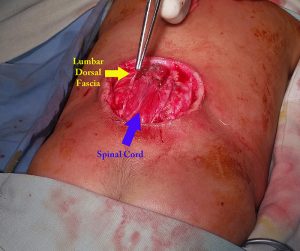
The dissection is done under loupe magnification. The neural elements are dissected free of the epithelium, fat, scar tissue, and fibrous bands. In the picture above the spinal cord with attached neural placode and the lumbar dorsal fascia have been identified.

In many cases the lumbar dorsal fascia can be carefully dissected at the lateral extant of the wound and then reflected medially to be closed as a dural layer. In the picture above this “dural” layer is closed first by several interrupted 3-0 vicryl sutures and the oversewn with a running suture.

Key to being able to close the wound is mobilizing the subcutaneous fascia superiorly and inferiorly and bilaterally. This must be generously done by careful digital dissection to free up the skin edges. It is generally better to over mobilize then undermobilize to reduce tension on the skin closure. If the a primary midline closure cannot be done then the primary skin fascial incision can be extended to superior and inferior z-plasty incisions which must be longer than the original incision. Alternatively a rhomboid type flap can also be used. It is important in the post-operative period to support the flap by giving supplemental oxygen, maintaining hydration, checking the post-operative hemoglobin/hematocrit, and avoid undo pressure on the flap. Most of the cases can be primarily closed.
Despite the best techniques, about 20 percent of cases have some type of wound problem which can range from mild stitch abscess or dehisicience to severe dehisicience. I always tell the surgical residents that we close the dura thinking that should the flap come apart with a sound dural closure we have a good chance for secondary healing.

This was a very large myelomeningocoel that we attempted to close with a modified z-plasty. Unfortunately a week after surgery there was some necrosis and breakdown. However, with aggressive daily wound care and good nutritional support a good result was obtained by secondary intention healing over a month’s time because of the good dural closure underneath.
Careful monitoring of the head circumference, anterior fontanel, eye movements, mental status, and feeding is necessary in the immediate and later post-operative period. Most of these children will go on to develop progressive hydrocephalus requiring a second operation for insertion of a ventricular peritoneal shunt. A few of them if they have persistent stridor, weak cry, aspiration will need to go undergo an upper cervical laminectomy and decompression of the brainstem for treatment of the Arnold-Chiari malformation.