The head injury problem especially that due to interpersonal violence in Tigray is a growing and significant problem which requires a public health approach.

Research published by Fasika et al showed that 24.8% of head injury admissions came from interpersonal violence from 2011 to 2014 which was before neurosurgery was permanently established at Ayder Comprehensive Specialized Hospital. Currently we are seeing about 10 patients a day and operating on 2 to 3 every day. Most of the surgeries we do are for depressed fractures caused by stone injury received in interpersonal violence. The age range of these injuries ranges from preschool to the eighth decade of life. We know there is a cultural proclivity to this type of injury but it is not well studied.
The hospital burden of head injury includes about 19% of adult ICU admissions and bedspace and 25% of pediatric ICU admissions and bed space. Our average daily census on the adult ward is 5 for head injury and on the pediatric ward also 5. The length of stay can vary from 24 hours to months with most of the surgical patients requiring a least a 5 days stay in the hospital.This burden acts to limit the care those suffering from other maladies can receive.
At the current time there is no public health or government plan to try to prevent these injuries.The World Health Organization has created a Violence Prevention Alliance which sees interpersonal violence as requiring a public health approach.
This public health approach to violence prevention seeks to improve the health and safety of all individuals by addressing underlying risk factors that increase the likelihood that an individual will become a victim or a perpetrator of violence.
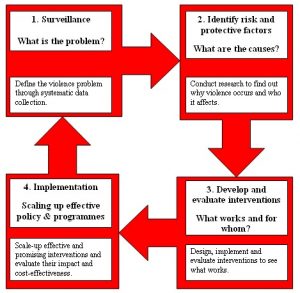
The approach consists of four steps:
1 To define the problem through the systematic collection of information about the magnitude, scope, characteristics and consequences of violence.
2 To establish why violence occurs using research to determine the causes and correlates of violence, the factors that increase or decrease the risk for violence, and the factors that could be modified through interventions.
3 To find out what works to prevent violence by designing, implementing and evaluating interventions.
4 To implement effective and promising interventions in a wide range of settings. The effects of these interventions on risk factors and the target outcome should be monitored, and their impact and cost-effectiveness should be evaluated.
By definition, public health aims to provide the maximum benefit for the largest number of people. Programs for the primary prevention of violence based on the public health approach are designed to expose a broad segment of a population to prevention measures and to reduce and prevent violence at a population-level.
I propose that Mekelle University put together a multidisciplinary team consisting of not only physicians but also social scientists, public health professionals, police and prosecutors ( this was previously discussed with the head of the Tigray police who was interested), and government stakeholders. This type of investigation and policy development is exactly the type of activity which the University with all its resources and knowledge base should be tackling.